Our Values: Evidence Based
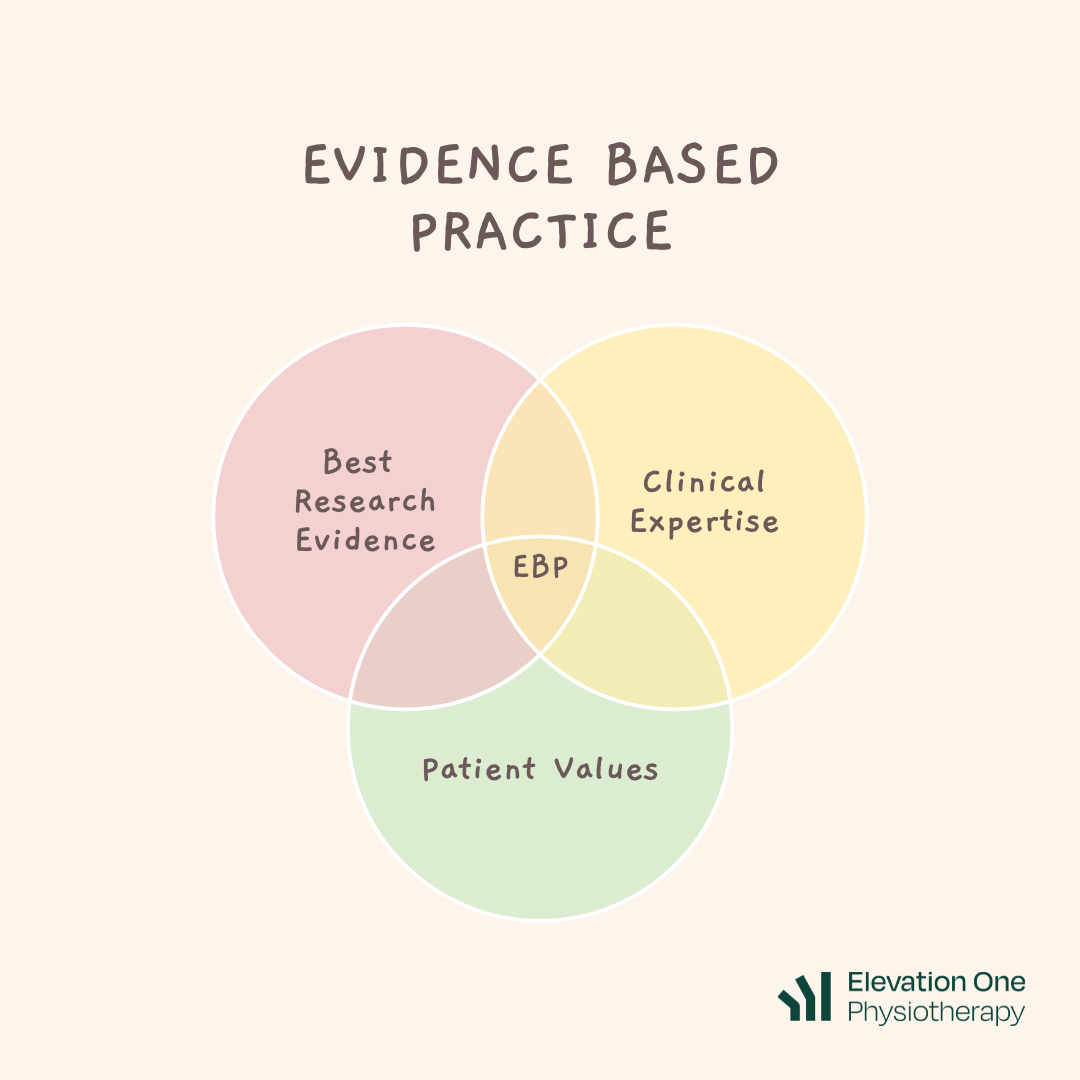
What is evidence based practice?
We think it’s really important to keep up to date with the most recent evidence and information so that we can provide the most effective treatments.
We then need to ask ourselves how what we’re reading/learning fits with our clinical expertise and experience of the real world, and pair that with what our patient’s values are. It’s the integration of these three pillars which gives us evidence based practice (EBP) [1].
This concept of EBP was brought about in the 90s, with the shift from “pathophysiological rationale” to scientific and clinically relevant research. Despite being around for so long though, we still often see mistakes with the way people approach EBP - which often occurs when there is a bit of bias towards a particular pillar.
Common mistakes:
“If it ain’t broke, don’t fix it”
With science being something that constantly evolves and develops, it’s easy to fall behind with current evidence. Sometimes this is quite obvious, where something is just just incredibly outdated. Other times, it’s a bit more subtle, because as creatures of habit we like doing things that we’ve “always done”. What happens is, the practitioner puts more/too much emphasis on the “Clinical expertise/experience” side of EBP, and begins to justify treatment using that pillar alone.
An example of this is the management of acute soft tissue injuries using the acronym RICE (rest, ice, compression, elevation). This actually isn’t used anymore in physiotherapy settings, and has had a few changes to the acronym over the years - from RICER to PRICE, to POLICE, and now to PEACE + LOVE (we’ll do a blog on this later).
The evidence extraordinaire
Conversely, there are times where practitioners can go the other way and have a bit too much bias on the “evidence” side of the EBP relationship. With all the new emerging evidence at our fingertips it seems only noble and right to let that dictate our practice. However, without understanding scientific evidence within the context of clinical expertise we can also fail to provide effective EBP treatment.
An example of this is when we see good scientific research but fail to understand how it translates (or rather how it doesn’t translate) to the clinical setting. It might be statistically significant when a joint is deviating 3mm from where it should be, but we need to understand the context of the study and whether it's reproducible and applicable for the general population. It’s all fun and games until we’re making an 80 year old perform a single leg hop test to see if her SIJ is in the same position that we saw in a paper for 16 year old professional ballet dancers!
[1] Sackett, D. L., Rosenberg, W. M., Gray, J. A., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: what it is and what it isn't. BMJ, 312(7023), 71–72. https://doi.org/10.1136/bmj.312.7023.71
This blog and the contents within are shared to enrich the understanding that members of the Elevation One community have in relation to physiotherapy and general health. It should not be used to diagnose any medical conditions and is not health advice. We always recommend seeking a medical professional for your health concerns.